Orthosis Fabrication
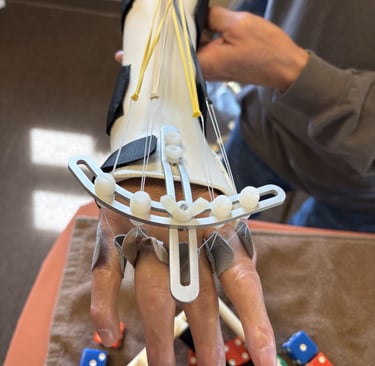
Splinting of the hand is the process of using thermoplastic material to fabricate a custom Orthosis based on your diagnosis needs. This skill is specific to therapists that specialize in the treatment of the upper extremity. The therapist should be knowledgeable of anatomical principles, how tissue heals and scar tissue matures, how to apply mechanical principles to the orthotic design to achieve desired effects, and be skilled in handling the material and tools so as not to apply areas of pressure, which could potentially cause tissue breakdown. But, most importantly the therapist must be able to evaluate and determine the appropriate design of the orthosis that suits the patient's diagnosis requiring the need for rest, soft tissue modification, joint mobility and corrective mechanics.
I have 30 years of experience and have completed several continuing educational courses from beginning to advanced fabrication of orthosis. I will design, fabricate, fit, adjust and describe the billing associated with orthosis fabrication. Also, there is the reevaluating process of how effective the orthosis intervention is for you, which will be monitored throughout your treatment use of the orthosis.
I am very comfortable using patterns to fabricate an orthosis for you, but also well versed in designing my own patterns to suit your needs. I am comfortable manipulating the material with an artistic background, it's actually one of the reasons I wanted to specialize in hand therapy because of the creativity in making orthosis. Throughout my 30 years I have learned on-the-job tips and tricks to be efficient in fabrication and to improve patient’s comfort to be successful in using the orthosis.






Neural Mobilization
Neural Mobilization or Manual Therapy of the Nervous System is a series of physical movements both passive and active. This technique focuses on the nervous system to decrease sensitization and facilitate movement of the nervous system to enhance pain relief and improve function in patients.
If you have been diagnosed with Carpal Tunnel Syndrome, Cubital Tunnel Syndrome, or Radial Tunnel Syndrome, which would involve one of these nerves, the median, ulnar or radial nerve. You are then someone who would benefit from neural mobilization.
Visualize the nerves moving through “canals” (surrounding tissue or spaces), when nerves are moving, also called gliding they are “happy” if a “dam” (space confinement) occurs in that canal then it restricts movement of the nerve, and nothing is feeding (blood flow) into or moving out in that canal, so you have a build up or blockage (swelling or scar adhesion) on the nerve resulting in symptoms a “unhappy” nerve.
Three factors are important for nerves to be “happy” they need to have (1) SPACE to be able to (2) MOVE within the space, and through movement increase (3) BLOOD FLOW.
Nerves travel through the body and adapt to surrounding tissues, nerves need to freely move through these surrounding tissue spaces. If the space they are moving through becomes blocked by a “dam in the canal”, then this limits them from moving/gliding, resulting in decreased blood flow to them and “unhappy” nerves.
There are several spaces in the upper extremity where entrapment of the nerve can occur and also in the cervical area. In my evaluation we will look to identify areas of space confinement secondary to muscle tightness, swelling/edema, scar adhesion's, fascia restrictions and a mechanical stress through poor sleeping posture or habits
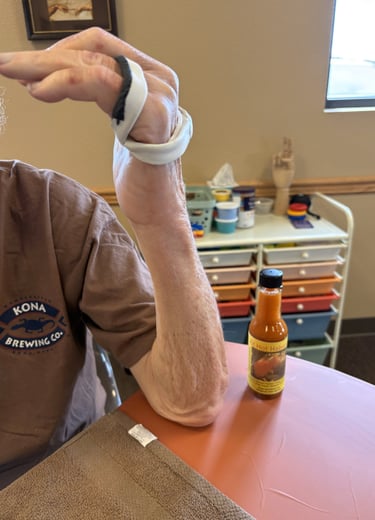
Treatment to open up the space consists of upper extremity stretches, ROM, postural re-education, neural mobilization passively (manual techniques performed by therapist) and active nerve gliding (your home exercise program), and a night brace. The brace is to modify your sleeping posture to prevent you from compressing and decreasing the space that the nerve flows through that is causing symptoms. Movement, humans are not meant to be stationary, everything must move/glide. Through nerve gliding exercises both passive and active, you are gliding the nerve through its normal pathway. By gliding the nerve you are preventing adhesion along the nerve that would restrict its movement. You are also helping to flush swelling/edema surrounding the nerve away that could be creating that “dam” and causing symptoms. Blood flow created by movement and getting to the nerve by the space being open provides nourishment to the nerves to be “happy.” Blood flow must be pushed towards the nerves to feed them, also blood flow helps to push waste products out to leave the area and open that space.
Manual Therapy of the Nervous System facilitates nerve gliding, it is a very effective tool along with other treatment techniques provided, and patient’s compliance in their home exercises program to create “happy” nerves resulting in a decrease or elimination of their symptoms.
I now reference a testimonial from Joe Short, one of my patients I treated with Neural Mobilization on my web page




I recently finished 10 weeks of hand therapy with Laura Visanko at Millennium. Laura has treated me twice before when she was with another company, both times for therapy to recover from Arthroscopic Surgery. A few months ago, I was considering surgery for Carpal Tunnel Syndrome. I asked my family doctor if she thought therapy might be an alternative for surgery. She thought I was a good candidate for a therapeutic recovery and sent me to Laura (at my request). I spent 10 weeks with Laura, 2 sessions per week. After 10 weeks, my symptoms were reduced to about 10% of their original level. I continued the home program Laura designed for me after I was discharged. 45 days after discharge, I am 100% recovered. I met my goal of avoiding surgery. I recommend Laura highly! I have been her patient 3 times over the last 10 years and I would not use another hand therapist. If you have hand problems, ask your physician for a referral to Laura. She is the best. Joe Short


Trigger Finger
Stenosing Tenosynovitis, also known as a Trigger Finger, is very common. Hand therapy may assist in a reduction or resolution of symptoms.
A trigger finger involves the pulleys and flexor tendons of the fingers that bend the fingers. These tendons and their sheaths run through pulleys in the hand. There are 5 pulleys in each of the fingers, the most important two are A2 and A4.
The A1 pulley is the pulley most susceptible to inflammation resulting in catching or locking of the finger as it bends. The pulleys hold the tendons proximal to the bones, and acts as a tunnel for the tendons and sheath to glide through during range of motion to make a fist and straighten your fingers. Inflammation may occur through repetitive use, sustained and/or resistive tight composite flexion gripping. It is also very common in people who are diabetics, having multiple trigger fingers.
The pulley may become inflamed and the space narrows for the tendon and sheath to glide through, or there may be inflammation of the tendon sheath making it harder for the tendon to glide through the pulley, or both. In a properly functioning hand, the tendon gliding in the sheath is very fluid. There is little or no resistance to tendon movement, as if moving through water. If inflammation occurs, the tendon is "moving through molasses" so to speak, and the sheath is thicker and swollen. You can palpate (feel) tendon crepitus “crunchies” as the tendon glides and it may be tender to the touch. You may also feel a nodule that clicks as it goes through the pulley. This may be a secondary effect of the condition with a calcium build up, but is not the primary cause of a trigger finger. The inflammation of the pulley and swelling of the tendon sheath are the primary causes, and this will restrict tendon movement resulting in a trigger finger.
Treatment through hand therapy is most effective in treating trigger finger when it is initiated at the first notice of symptoms. Most people will wait until the finger is locked before seeking treatment, making recovery from the trigger finger more difficult. Cortisone injections are one form of treatment provided, but may only mask the pain for a short period of time. If caught early the best hand therapy treatment is educating the patient on their condition, activity modification by avoiding sustained composite flexion and building up the handles of their tools to decrease grip force. Also, resting through immobilization, tendon gliding to promote movement of the tendon through the pulleys to prevent adhesion developing along the tendon, movement to flush swelling out and increase the space, and movement to increase blood flow to provide nutrients for healing.
Recovery after surgical trigger finger release begins again through educating the patient on their condition, managing swelling/edema, modification of scar tissue and facilitating tendon gliding to restore ROM and function of the patient.
Thumb Osteoarthritis
Thumb Osteoarthritis of the Carpalmetacarpal joint (CMCJ) is a result of degenerative changes on the trapezium and the base of the first metacarpal. This joint is predisposed to arthritic changes because of its design and structure. The joint capsule is loose and the joint surfaces are not equal in size and shape, giving the thumb more mobility and allowing us prehension patterns (pinching and gripping) to function. But, this design and structure also results in more wear and tear on the joint, which is then further exacerbated by poor mechanics.
There are four stages of thumb osteoarthritis (OA):
Pain in the CMCJ due to synovitis (inflammation of the tissue lining the inside of the joint)
The start of changes in the CMCJ because of OA.
The OA changes increase and there is bone crepitus, narrowing of the joint space with bone-on-bone grinding.
The OA further advances resulting in changes in appearance of the CMCJ and also begins to affect surrounding carpal bones the scaphoid.
There are factors that may make you more susceptible to OA of the CMCJ, such as a family history and your age. OA is more common in women than it is in men. How you use your hand is also another contributing factor. If you have poor mechanics with your hand during function and repeat these poor mechanics throughout your life, you may be contributing to the changes in the joint to include the ligaments and muscles that help support the joint. There are ligaments supporting the CMCJ and adjacent joint the Metacarpal Joint (MPJ) that provide stability during function of the thumb, but when there is ligament laxity and hypermobility this results in more wear and tear in the CMCJ. Also, when using your hand with poor mechanics, for example pinching with wrist flexion or ulnar deviation, you begin to use different muscles to perform those prehension patterns. This results in weakening the muscles that provide stability to the CMCJ. Through repetition, you continue strengthening the muscles that promote poor mechanics. This creates "muscle memory" of these OA patterns of movement, which can, over time, lead to OA changes in the thumb. These patterns include first metacarpal dorsal subluxation, hyperextension of the MPJ, thumb adduction and increased flexion and ulnar deviation of the wrist. Once these patterns are established they are difficult to change. In some people the OA changes have progressed to stage 4, where surgical intervention may be your only option to alleviate the pain. If caught early in stages 1 and 2 you have a good chance of managing your OA pain through hand therapy and education. In stage 3, hand therapy treatment can help you if your choice is to avoid surgery by teaching you techniques for pain reduction. My goal for you starts with educating you on your condition. Education begins with joint protection, teaching you proper mechanics of the thumb and wrist so you do not get into that cycle of creating poor muscle memory. I will teach you proper thumb AROM with proper wrist mechanics, Next I will work on strengthening your CMC and wrist stabilizers to support the CMCJ and improve your wrist mechanics. I will also instruct you on manual techniques for the thumb and wrist to assist in pain management. I will provide you with information on a thumb brace to promote rest for pain management and also a thumb brace to improve the mechanics of your thumb during function. These techniques and the education I provide are a lifestyle redesign, something you will have to continue doing through your lifetime. There is no easy fix and I can not change the OA that has already occurred to the CMCJ, but these techniques do work if you are invested in doing them. If the pain begins to limit you more significantly in function then you're a surgical candidate. I will give you information on the different surgical procedures out there that your hand physician may choose for you once he evaluates the stage of your OA. After surgery I will address patient education, edema/swelling management, scar tissue modification, AROM and the progression into appropriate functional strengthening.
I am truly passionate about this diagnosis, and love educating people about thumb CMC OA. I was invited to speak on this subject to the Las Cruces Knitting Guild and was also invited to speak at the Military Officers Association of America, Mesilla Valley Chapter.
I feel confident that I can provide you with information to help you learn to manage your OA pain if you are invested in learning.
